A revolutionary piece of news comes from Fudan University in Shanghai: researchers have developed an innovative artificial retina, based on the interweaving of tellurium nanowires. This extraordinary discovery has allowed blind mice to partially regain sight, marking a crucial step forward in the field of artificial vision. This project, which combines nanotechnology with ophthalmology, is a tangible hope for millions of patients suffering from retinal diseases that are currently incurable, offering innovative solutions for restoring sight.
The revolutionary approach of artificial retina
The human retina is a delicate layer of nervous tissue located at the back of the eye, responsible for the perception of images. In many degenerative diseases, including retinitis pigmentosa, age-related macular degeneration and other rare diseases, retinal cells undergo progressive death, leading to the loss of visual function.
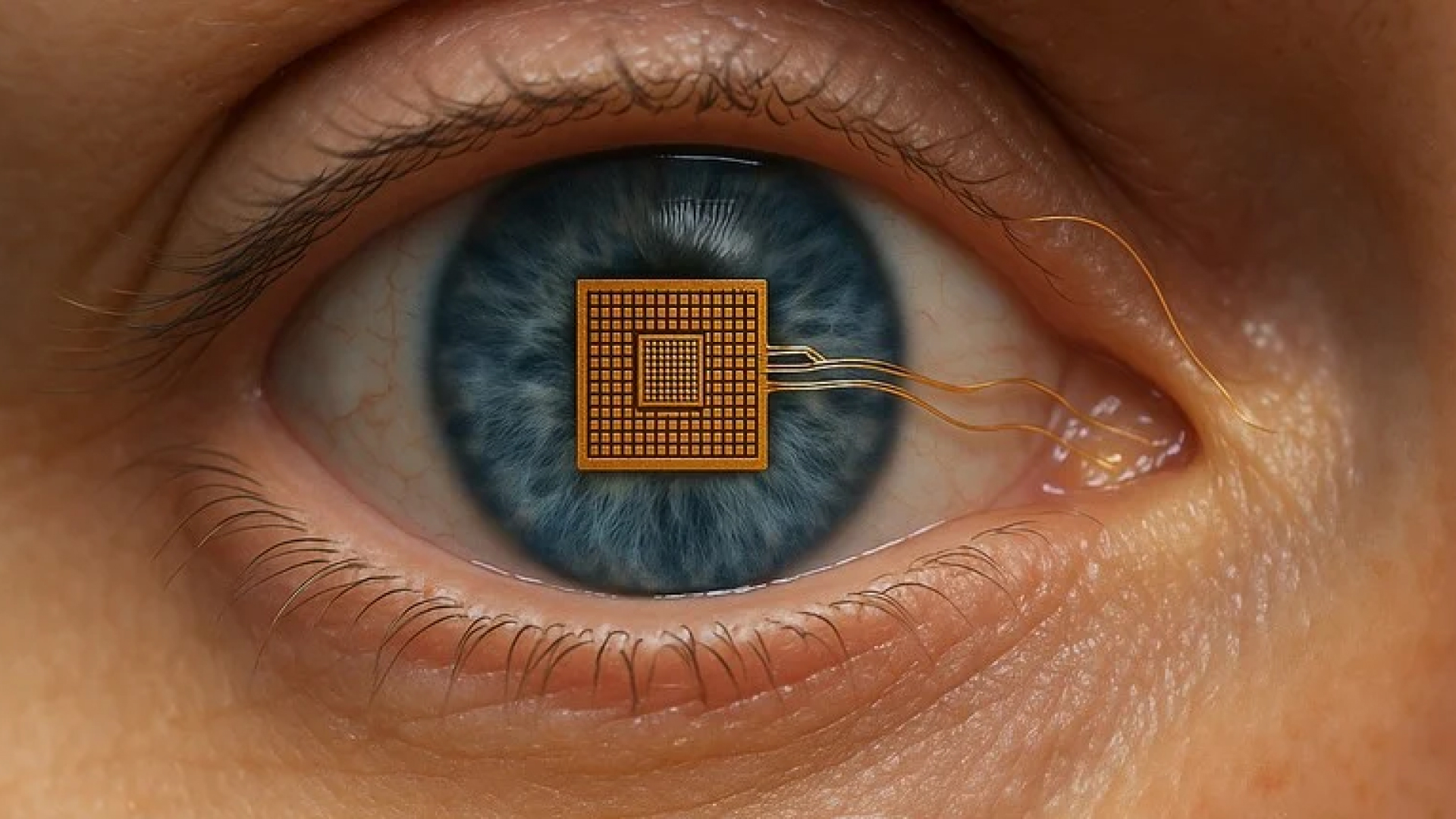
The artificial retina is a technique already previously used with Argus II, a technological device that uses electrode arrays to stimulate residual neurons. The approach used by Fudan University improves on this technique, exploiting the electrical charge generated by tellurium nanowires, semiconductor materials that, when exposed to light, create electrical signals that can be directly exploited by the central nervous system as visual impulses.
Tellurium nanowires are, in fact, the innovative element of the project because, as nanometric filaments intertwined with each other, they have optimal electrical and mechanical characteristics for implantation on the retina.
Human application perspectives
The success of the experiment on animal models opens up fascinating scenarios for the fight against the main degenerative diseases of the human retina.
Even partial restoration of visual function could have an extraordinary social and economic impact, drastically improving the quality of life and daily autonomy of affected individuals. However, researchers believe that further refinement of neural integration and control of the immune response is necessary to ensure safety, durability of the implant and absence of long-term complications.
Among the main challenges that have emerged are the long-term safety of the implant in human tissue, the complexity of the neuronal connection, the customization of the device to adapt to the anatomical and pathological diversity of patients, and the future financial accessibility of the public health system.
Further studies on more complex animal models and, subsequently, controlled clinical trials on small numbers of patients will be the next steps necessary to certify the validity and safety of the prostheses. No less important will be the integration of these technologies with artificial intelligence software capable of modulating the visual response in real time, laying the foundations for artificial vision technology.